Skene’s gland abscess: a rare case report
Muhammad AS1, Gabi UI2, Ja’afaru UH2, Kabir AM2
Abstract
Background: The Para urethral gland of Skene is a pair of glands in the vestibule on the distal two-thirds of the female urethra, they are homologous to the male prostate gland and are believed to secrete fluid that lubricates the urethral opening. They contain about 6 to 30 small glands. The grand’s duct can get infected and hence inflamed obstruct. The secretion may accumulate leading an abscess formation. The patients may develop fever, dysuria, or dyspareunia. On examination, there may be a visible palpable Para urethral mass which may be unilateral or bilateral, it may also be tender. The incidence of Skene’s gland abscess is unknown, it is common in premenopausal women usually in the third and fourth decades of life. Trans trans-perineal ultrasound scan is very useful in the diagnosis but MRI is the gold standard. An important differential diagnosis is urethral diverticulitis which can be distinguished using these imaging modalities.
Case report: We present a 30 years old nulliparous single lady who had a 2-year history of vaginal swelling and superficial dyspareunia we made a final diagnosis of palpable skene’s gland abscess, which was treated by marsupialization.
Keywords: Skene’s gland abscess, male prostate, superficial dyspareunia
Introduction
Para urethral glands or skene’s glands are a pair of glands situated on either side at the distal two-thirds of the female urethra, mainly in the dorsal and lateral mucosal stromal tissue. It was first discovered by a Scottish Gynecologist in 1880 Alexander Skene.1 Skene’s gland abscess is a rare occurrence with significant morbidity and even mortality if left untreated. The gland may secrete prostate-specific antigen and prostatic acid phosphatase. Cysts of the gland are less common and when infected can become an abscess.2 The patient may present with painful micturition, painful sexual intercourse, or vaginal discharge, and on examination, a palpable tender mass or masses (in case of bilateral abscess) may be felt at caudal two third of the urethra. We present a case of a 30 years old single lady with a 2 years history of a mass in the vagina and superficial dyspareunia.

Fig. 1: The above figure shows the right skene’s gland before marsupialization
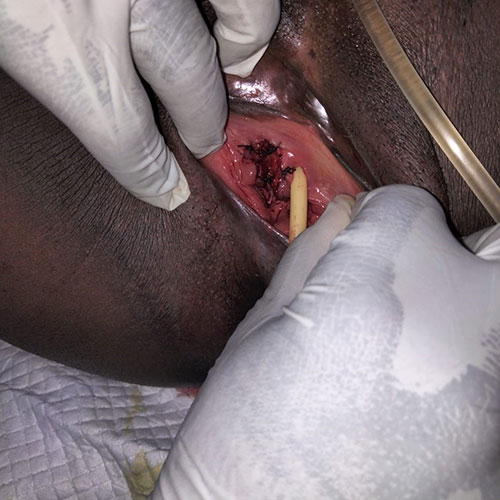
Fig. 2: Shows the right Skene’s gland after Marsupialization
Case report
The patient was a 30-year-old single nulliparous woman who was sexually active and had a regular monthly menstrual period. She presented to our gynae clinic with a 2-year history of palpable mass in the upper vagina and superficial dyspareunia, there was no history of fever, but has a history of use of antibiotics from specialist hospital Bauchi with no improvement. On examination, she was a young lady calm, weighing 85kg. Her height was 1.8m, which gives a BMI of 26kg/m2. She was afebrile with an axillary temperature of 37.00 C. All vital signs were stable, and vaginal examination revealed poor perineal hygiene, and an ovoid brownish mass on the right distal end of the urethra was seen, it was fluctuant and tender, measuring about 3cm by 4cm. The urethra was shifted to the left side by the bulging mass. Laboratory investigation revealed a negative retroviral screening test and hepatitis B, hematocrit of 34.6%, and WBC and neutrophil counts were normal. A transperineal ultrasound scan revealed a loculated inhomogeneous cystic mass on the right side of the urethra measuring about 33mm by 45mm, there was no communication between the cyst and the urethra. A conclusive diagnosis of Skene’s gland abscess was entertained, and the findings and the method of treatment were explained to the patient. She was planned for marsupialization in the theater. Under saddle block, she was placed in a lithotomy position, and she was cleaned and draped, a urethral catheter attached to a urine bag was inserted and left in situ. With the aid of an assistant, two sim’s specula were gently inserted in the vagina, one to distend the posterior vaginal wall and the other to distend the right lateral vaginal wall. A two-centimeter longitudinal incision was given on the cyst, wall opening the cyst cavity, a brownish effluent was drained, a pus sample was collected using a 5cc syringe for MCS, a urine sample from the urine bag was also collected for MCS., and tissue was also taken from the cyst wall for histology. The cyst wall was everted and using a Vicryl 20 suture, the everted cyst wall was sutured to the vaginal mucosa at intervals enough to keep the cyst cavity opened. She was placed on parenteral antibiotics and analgesics, and after recovery from anesthesia, she was transferred to the gynae ward. She was observed thereafter and discharged after 24 hours on perineal hygiene and abstained from sexual intercourse until the wound healed, her drugs were converted to oral, and the urethral catheter was removed. She was given an appointment at the Gynae clinic to be seen after 1 week with urine and pus MCS including the histology results. At the clinic, there was no complaint from the patient, and she had completed her oral drugs, Urine MCS result revealed no pathogen, but pus MCS revealed Escherichia coli sensitive to one of the antibiotics the patient was placed on. The histology result revealed a section of tissue composed of partly denuded epithelial lining composed of pseudostratified columnar epithelial cells. The fibrous stroma is composed of a few tubular glands. Other areas show hemorrhage and sprinkles of inflammatory cells. The findings were explained to the patient and was given six-week appointment. The patient was seen again at the gynae clinic, she had no complaint and had resumed coitus. The patient was counseled on perineal hygiene and was discharged from the clinic.
Discussion
Skene’s glands are a pair of glands that were first described by Regnier de Graaf (1641–1693) but were named after the Scottish gynecologist Alexander Skene, who published his findings in 1880. The Skene’s glands, or Para urethral glands, are found in the distal two-thirds of the urethra, mainly in the dorsal and lateral mucosal stroma. They originated from the urogenital sinus, they are located downward and on the two sides of the urethra, close to the urethral opening. The main drainage of the gland opens on either side of the urethra. They are termed, the female homologous of the prostate gland,3 they are not present in all women but only two-thirds, and may play a role in female ejaculation. Skene’s gland abscesses are most commonly present in women between thirty and forty years of age, and it is uncommon to find Skene’s gland abscesses in children. Most cases of Skene’s gland abscess occur without predisposing risks, but some risk factors may include: diabetes, obesity, being pregnant, accidents involving the genital area, and poor genital hygiene,4 leading to high chances of infections (this is the only risk factor identified in our patient). Presenting symptoms of Para urethral gland abscess are lower urinary symptoms, dyspareunia, presence of a mass in the upper vagina, recurrent lower UTI symptoms, and urethral discharge. Our patient presented with dyspareunia and a mass in the upper vagina.5 Fifty percent of the paraurethral gland abscess can be palpable. The diagnosis is based on the history, physical examination, laboratory, and radiological evaluations. A history of risk factors and symptoms as described above can be sought. And on genital examination, the anterior vaginal wall and an area along the urethra should be checked for masses or points of tenderness. Diagnosis, of patients with non-palpable skene’s gland abscess, can be challenging requiring more sophisticated imaging modalities.6 In patients with chronic lower UTI symptoms, unexplained pain during sexual intercourse, is a diagnostic dilemma but paraurethral gland abscess can be a differential. Pain at sexual intercourse and micturition are the most common presenting symptoms (our patient had dyspareunia).7 Skene’s gland abscess is always at the anterior vaginal wall, at the symphysis pubis level, and Para median to the urethra. During the USS examination of a woman with UTI symptoms presence of fluid, (homogeneous in case of cysts or inhomogeneous in case of abscess), and para urethral mass, may suggest the diagnosis of Skene’s gland cyst or abscess.8 Our patient had an inhomogeneous fluid collection in the Skene’s gland, this favors the diagnosis of paraurethral abscess. Voiding cystourethrogram and double-balloon urethrogram are also options for diagnosis, but Magnetic resonance imaging is noted to be superior. Hence Preoperative MRI is used in challenging cases for urethral diverticulum. Magnetic resonance imaging was not done in our patient because MRI is not available in our center and the diagnosis was not challenging. Infection of the paraurethral gland is termed skenitis, and recurrent infections may lead to obstruction of the gland and result in a suburethral cyst or even an abscess cavity as seen in our patient. Extensive paraurethral gland cysts or abscesses may cause urethral obstruction and even urinary retention. Bacteria associated with a Skene’s gland abscess include Escherichia coli (as seen in our patient). Neisseria gonorrhoeae, vaginal flora, and other coliform bacteria.9 Antibiotic therapy is typically initiated to cover these common bacteria. If there is no response to antibiotics, then surgical therapy is offered as is the case with our patients. Surgical management can be instituted in cases of recurrence following one or two courses of antibiotics. There is no general agreement on the specific surgical treatment of paraurethral gland abscess, some modalities may include: Skene’s gland enucleation, marsupialization, and incision and drainage. Spontaneous drainage has also been reported.10
The frequency of Skene gland abscesses may be under-reported, they can be detected during the evaluation of women's lower urinary tract symptoms unresponsive to treatment or urological procedures.11 Skene’s gland abscess may simulate genital malignancy, urethral prolapse, or diverticulum, others are ureterocele, Bartholin cyst, Gartner's duct cyst or abscess.12 In the case of an infected Skene's gland, conservative therapy with antibiotics is the first-line therapy, this was done to our patient but did not yield any significant recovery hence she had the surgery.3 Furthermore, a neglected infected paraurethral gland abscess may lead to serious complications such as a urethral diverticulum.
Conclusion
Paraurethral gland abscess incidence is unknown, however, the condition may be under-reported due to misdiagnosis, hence adequate clinical skills and appropriate laboratory and radiological investigations are of utmost importance in the diagnosis and treatment of this condition to reduce its complications.
Declaration of Patient Consent
We certify that appropriate consent forms were filled. She consented that her clinical information including images can be used in journals. She understood that efforts will be made to conceal her identity and that her name or initials will not be published, but anonymity cannot be guaranteed.
Financial Support and Sponsorship: Nil
No conflict of interest.
References
- Pai M, Kushtagi P, Chakravarti SU. Manual of Obstetrics E-book. Elsevier Health Sciences; 2015 Oct 15.
- Al-Shaiji TF, Al-Otaibi K, Malallah M, Zohair M, Al-Mansouri MM. Acute Urinary Retention Secondary to Skene’s Gland Cyst: A Case Report. J Urol Ren Dis. 2021;6:1229.
- Tamburrini S, Vascone C, Marrone V, Catalano M, Del Biondo D, Gallo L, et al. Skene's glands abscess an overlooked diagnosis in acute lower urinary symptoms. Radiology Case Reports. 2021 Dec 1;16(12):3751-6.
- Gomes de MA, Reuter MF. Profile of Antimicrobial Resistance and Sensitivity in Vulvar Abscesses in Women Attending a Tertiary Hospital. Gynecol Reprod Health. 2022; 6 (5): 1-4.
- Kulkarni M, Rosamilia A. Common Urethral and Vaginal Lesions in Ambulatory Urogynaecology. Ambulatory Urology and Urogynaecology. 2021 Jan 20:109-22.
- Gillor M, Dietz HP. Translabial ultrasound imaging of urethral diverticula. Ultrasound in Obstetrics & Gynecology. 2019 Oct;54(4):552-6.
- Yayla D, Demıtas G, Tagcı S, Karabulut B, Tıryakı HT. Paraurethral Skene's cyst case in puberty. Journal of Pediatric Surgery Case Reports. 2021 May 1;68:101788.
- Matos J, Orazi C, Sertorio F, Magnano G, Toma P, Granata C. Imaging of diseases of the vagina and external genitalia in children. Pediatric Radiology. 2019 May 1;49:827-34.
- Sushma BN. Microbiological Profile in Women with Symptomatic Vaginal Discharge (Doctoral dissertation, Rajiv Gandhi University of Health Sciences (India)).
- Vulva V, Cervix U, Oviduct O. 18 Benign Gynecologic Lesions. Comprehensive Gynecology. 2021 May 8:362.
- Kassa ZY, Hussen S, Hadra N, Moges Y, Bonja F. Prevalence of Neisseria gonorrhoeae infection among women of reproductive age in sub-Saharan Africa: a systematic review and meta-analysis. The European Journal of Contraception & Reproductive Health Care. 2020 Sep 2;25(5):365-71.
- Berechet MC, Nacer K, Bumbu G, Maghiar TA, Bratu OG, Tica O, et al. Skene Duct Abscess–Case Report. Romanian Journal of Urology. 2021 Oct 1;20(4):60-5.