An aberrant right subclavian artery in a chronic obstructive airway disease patient
Elendu KC1, Chima E2, Uwanuruochi K3
Abstract
Background: A seventy-six year old man, known hypertensive, presented with chest pain of five years duration, associated with exertional breathlessness, wheeze, cough, leg swelling and fatigue. His chest radiograph showed signs of hyperinflation, and chest computer tomography showed an aberrant right subclavian artery. We discuss the implications of this finding to diagnosis, and clinical management.
Key words: Chronic obstructive airway disease, chest pain, aberrant right subclavian artery.
Key Message: We present a elderly man on management for chronic obstructive airway disease, in whom an aberrant right subsclavian artery was discovered in the course of investigations. We discuss implications in his management.
Case report
A 76-year-old male presented to the clinic with history chest pain for five years. It was left parasternal in location, non-radiating, gradual in onset but increasing in intensity, aggravated by exertion and relieved at rest, associated with progressive exertional shortness of breath, fatigue, wheeze, cough that is triggered by exposure to dust, and leg swelling. He did not have orthopnea, and was hypertensive for more than twenty years, being treated with amlodipine and hydrochlorothiazide. He had asthmatic symptoms with exposure to rugs but that had subsided for ten years. He also had diabetes for three years, and was on treatment for benign prostatic hypertrophy. He took two sticks of cigarettes for five years during his youth.
He was in distress, anicteric and acyanotic. His pulse rate was 96 beats per minute, respiration was 20/minute, oxygen saturation of 85% in the right arm, blood pressure was 130/70 mmHg. Hepatic and cardiac dullness were attenuated and breath sound were vesicular. An impression of chronic obstructive airway disease with well controlled hypertension was made and he was continued on amlodipine 10mg daily, clopidogrel 75mg daily with simple analgesics Codeine 8mg twice daily, paracetamol 500 mg twice daily.
He returned to the clinic with laboratory results. Chest radiograph showed hyperinflation. Erythrocyte sedimentation rate was 53mm/hour, hemoglobin concentration was 14.0 g/dl, and white blood count was 6400/µ, with monocytes 15.8%. Glomerular filtration ratio was 74 ml/min/1.73m2. Abdominal ultrasound findings were normal. On chest computer tomography there was no lung lesion, but on examining vascular structures, an aberrant right subclavian artery was noted (Figure1). The aortic arch measured 2.6cm, and the main pulmonary artery 2.7cm. Calcifications were seen in walls of the thoracic aorta and the aberrant subclavian artery. Echocardiography showed diastolic dysfunction and concentric ventricular hypertrophy.
Discussion
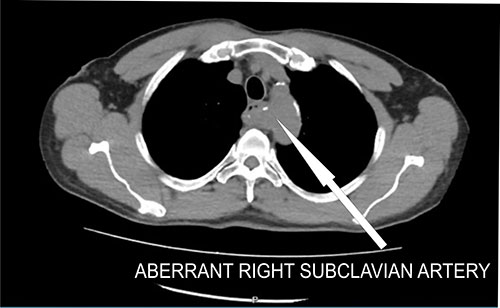
Figure 1: Computed tomography scan of aberrant right subclavian artery posterior to trachea
An aberrant subclavian artery has been recognized as a rare abnormality of the aortic arch,1 asymptomatic in most cases, but could cause dysphagia and heartburn by esophageal compression, or development of an aneurysm. It can also present with cough, chest pain, stridor, breathlessness, pneumonia (by compressing the trachea),2,3 and must therefore be considered in the differential diagnosis of cough in patients.
The anomaly can be associated with atherosclerosis changes, causes dilation, dissection, and therefore compression effects in surrounding organs.4,5 This may contribute to chest pain in our patient. With many cardiovascular risk factors, ischemic heart disease appears the most likely explanation for his pains, considering the location and associations.
He had been managed for asthma, but in the recent presentation, was diagnosed of chronic obstructive airway disease. This can explain desaturation. Cardiac anomalies may however be associated with other congenital defects. Differential cyanosis suggests congenital heart defects. The patient showed desaturation in the right arm, but saturation was not measured in the lower limbs to ascertain differential cyanosis. Measuring the oxygen saturation in both upper and lower extremities is recommended.6 This was however not done when the patient was reviewed. Echocardiography is also recommended when this abnormality is detected.
The finding of an aberrant subclavian artery will question the diagnosis for chronic obstructive airway disease, as the anomaly can present similar symptoms with the compression of the trachea. The history of smoking supports chronic obstructive airway disease. It is likely compression of the trachea and chronic inflammation both contributed to his ailment. He appeared to also have heart failure, most probably from cor pulmonale (from chronic obstructive airway disease) and hypertensive heart disease.
References
- Mahmodlou R, Sepehrvand N, Hatami S. Aberrant Right Subclavian Artery: A Life-threatening Anomaly that should be considered during Esophagectomy. J Surg Tech Case Rep. 2014 Jul-Dec;6(2):61-3.
- Polguj M, Chrzanowski Ł, Kasprzak JD, Stefańczyk L, Topol M, Majos A. The aberrant right subclavian artery (arteria lusoria): the morphological and clinical aspects of one of the most important variations--a systematic study of 141 reports. Scientific World Journal. 2014;2014:292734. doi: 10.1155/2014/292734. Epub 2014 Jul 1. PMID: 25105156; PMCID: PMC4102086.
- Massaro N, Verro B, Greco G, Saraniti C. Dyspnea in Patient with Arteria Lusoria: A Case Report. Iran J Otorhinolaryngol. 2020 Sep;32(112):333-336.
- Noaparast M, Samimi S, Pourhaji F, delshad M. h, Zebaradst J. The Relationship between Chest Pain and Right Aortic Arch with Left Aberrant Subclavian Artery. Ijmpp 2019; 4(2): 186-191. 2019; 4(2): 186-191.
- Taylor M, Harris KA, Casson AG, DeRose G, Jamieson. Dysphagia lusoria: extrathoracic surgical management. Can J Surg. 1996;39:48–52.
- Igawa Y, Watanabe Y, Murase M, Fujii T, Ikeda H. Interrupted aortic arch without differential cyanosis due to aberrant subclavian artery. Showa Univ J Med Sci. December 2022;34 (4), 221-224