Prevalence and pattern of sleep problems among older persons attending a tertiary hospital in Nigeria
Akinola OA, Etukumana EA, Morgan UOM
Abstract
Background: Sleep disturbances are common symptoms in adults and are related to various factors, but they are not an inherent part of the ageing process.
Objective: To determine the prevalence and pattern of sleep problems among older persons attending the General Out-patient Clinics in a tertiary health-care facility in Uyo, Nigeria.
Materials and Methods: This was a hospital-based cross-sectional descriptive study on older persons attending the GOP clinics of the University of Uyo Teaching Hospital. Using a semi-structured interviewer administered questionnaire, information on the sociodemographic characteristics and the sleep history of the respondents were obtained. Data entry and analysis were done using Epi info® version 3.5.1.
Results: The prevalence of sleep problems was 64.5% with early awakening being the commonest sleep problem (50.5%) experienced by the respondents.
Conclusion: The prevalence of sleep problems is high in this study, and there is need for counselling of older persons on how to improve their sleeping habits.
Key words: Sleep problems, older persons, Uyo
Introduction
Sleep is a natural phenomenon considered as one of the basic physiological needs of humans.1 It is a dynamic and highly organized biological process encompassing one-third of the human life.1 When a person sleeps, the body is put in a state of rest or hibernation which relates to the definition of sleep “as an active, repetitive and reversible neuro-behavioral state of relative perceptual disengagement from, and unresponsiveness to the enviroment”.2 Sleep is typically accompanied (in humans) by postural recumbence, behavioral quiescence, and closed eyes.2 Normal healthy sleep is characterized by sufficient duration, good quality, appropriate timing and regularity, and the absence of sleep disturbances and disorders.3,4
Over the last two decades, there has been an increased interest in understanding the biology of sleep and how it affects the human body, as well as a renewed focus on investigating factors influencing sleep. This is not unconnected with the fact that problems with sleep are widely prevalent and include deficits in quantity and quality of sleep.3 Sleep as a vital physiologic process with important restorative functions is essential for optimal day functioning, and it is not a homogenous process.4,5 As opposed to the general thinking that the reduced physical activity that sleep induces is related to a cessation of brain activity, sleep is considered to be responsible for reorganization of neural activity which ensures that many repair and restorative processes required for normal brain functioning takes place.6-8
Problems with sleep are widely prevalent and include deficits in quantity and quality of sleep.3 There are different sleep disorder classifications, however they are typically manifested in one of the following three ways: failure to obtain the necessary amount or quality of sleep (sleep deprivation), an inability to maintain sleep continuity (disrupted sleep, insomnia), and events that occur during sleep (e.g. sleep apnea, restless legs syndrome).3
An elderly person is an older individual with chronological age of 60 years or over as defined by the United Nations (UN).9 According to the UN, there are 901 million people aged 60 years or over, comprising 12% of the global population.9 Sleep patterns which are known to change across the lifespan in various ways can ultimately affect the quality of life of many older adults.10-13 With the growing population of older persons, the importance of sleep for the overall health and well-being of the elderly has been increasingly recognized as studies have indicated that about half of the older adult population experiences sleep disturbances.14 In the elderly, sleep patterns and distribution undergo significant quantitative and qualitative changes with up to 50% of older adults reporting difficulties in initiating and / or maintaining sleep.10-13 These changes in sleep architecture can be viewed as making older adults more vulnerable to sleep disturbances.13 Therefore, this study was aimed at determining the prevalence and pattern of sleep problems among older persons attending the General Out-patient Clinics in a tertiary health-care facility in Uyo, Nigeria.
Materials and Methods
This study was conducted at the General Outpatient Clinic (GOPC) of the University of Uyo Teaching Hospital (UUTH), Uyo, a major city in the southern part of Nigeria (specifically the South-South geopolitical zone). The study population included a sample of older persons aged 60 years and above who attended the General Outpatient Clinic for various medical problems during the period of study. Participants were of both sexes and came from either urban or rural communities in Akwa Ibom State and its environs. The GOPC has an average attendance of 13 elderly patients daily which translates to approximately 845 patients seen in the 13-weeks study period (i.e., approximately 13 patients daily, making 65 patients weekly and totaling 845 patients in 13 weeks). Patients aged 60 years and above who attended the General outpatient clinic of the University of Uyo Teaching Hospital, Uyo and gave informed consent were included in the study. Excluded from the study were patients that were acutely ill at the time of data collection, patients with cognitive dysfunction and patients who worked at night / do night shifts.
Estimation of sample size: Using the Leslie Kish’s sample size determination formula for cross-sectional studies,15 a prevalence rate of 75.4% of poor sleep quality among elderly individuals as reported by Awokola et al.16, a confidence level of 95% and a degree of accuracy (margin of error) of 5%, the sample size for this study was 214.
Sampling technique: A systematic sampling technique was used for this study. The sampling interval (K) was determined using the formula below:
K=N/n, where: N = estimated population size for study period = 845, and n = minimum sample size = 214
K=845/214 =3.95 =4
On each clinic day, the first subject was selected by simple random selection from the first four patients who met the inclusion criteria. This was done by asking respondents to pick from a basket containing four folded papers labeled with numbers 1 to 4. The subject who picked the number 1 was taken as the first respondent. A sampling interval of 4 was used for the study which implied that every fourth patient following the randomly selected first patient was recruited into the study. Participants were recruited during the working days (Monday to Friday) until the sample size was attained. To ensure that patients were not recruited multiple times when they visited the clinic more than once during the period of the study, the researcher exercised care by unobtrusively marking of each patient’s hospital folder following recruitment. Furthermore, the researcher kept records of recruited participants so that no participant was selected more than once.
The questionnaires were pretested among 22 patients at another General Outpatient Clinic of St. Luke’s Hospital, Anua, Uyo. Two research assistants were recruited and trained to assist with the administration of the questionnaire to the non-English speaking respondents.
Ethical considerations: Ethical clearance for the study was obtained from the Health, Research and Ethics Committee of UUTH, Uyo before the commencement of the study. Informed consent was obtained from the participants after the objective of the study had been clearly explained to them. Participation was voluntary with the option to decline without compromising their quality of care. Patients’ confidentiality was ensured.
Data collection: The instruments used for the study were: a semi-structured interviewer administered questionnaire which sought information on the sociodemographic characteristics of the respondents. It also obtained information on sleep history of the respondents. Specifically, respondents were asked if they had: “difficulty in initiating sleep”, “difficulty maintaining sleep”, “early awakening with inability to sleep back”, “tiredness or fatigue after sleep” and “difficulty staying alert during the day”. Respondents were required to give a yes or no answer to each of these questions. The diagnosis of sleep problem was based on at least one positive response to any of the questions listed above.
Data analysis: Data entry and analysis were done using Epi info® version 3.5.1. Descriptive statistic such as mean and standard deviation were used to analyze continuous variables while frequency and percentages of categorical variables were also determined.
Results
Sociodemographic characteristics of study participants
The sociodemographic characteristics of the study subjects are as shown in Table 1. Of the 214 subjects enrolled in the study, 110 (51.4%) were males, while 104 (48.6%) of them were females. The minimum age was 60 years and maximum age was 89 years. The mean age of participants was 66.8years (SD ± 5.7).
Table 1: Sociodemographic Characteristics of the study participants (N = 214)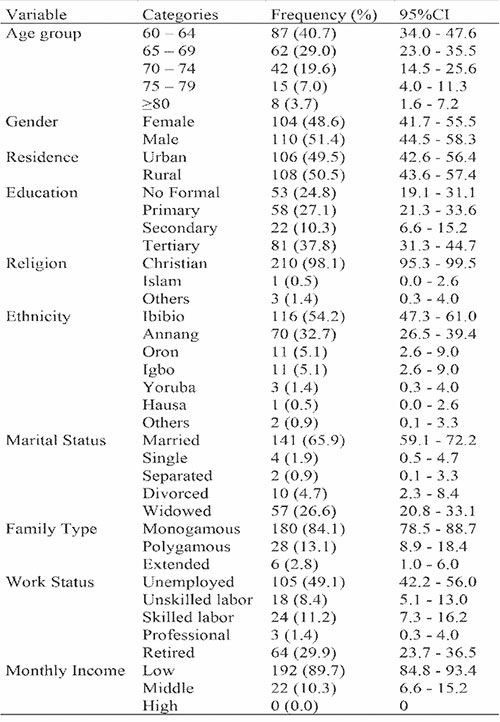
Prevalence and pattern of sleep problems in the study participants
One hundred and thirty-eight respondents (64.5%) had sleep problems. The pattern of sleep problems is as shown in Table 2. Early awakening was the commonest sleep problem in nearly half of the study participants with a frequency of 108 (50.5%), followed by difficulty in initiating sleep and trouble maintaining sleep 89 (41.6%) each. However, the least sleep problem was difficulty staying awake (35.5%).
Table 2: Pattern of sleep problems in the study participants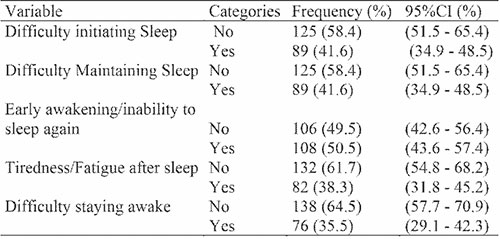
Discussion
This hospital-based study was carried out among 214 elderly subjects with a male preponderance. About 51.4% subjects were males, while 48.6% of them were females. The finding of male preponderance in this study is slightly higher than the figure recorded by Megbelayin et al. where 50.5% of patients presenting at primary healthcare facility in Uyo were males.17 This was however different from the finding of Adewole et al. in a study conducted in South-West Nigeria.18 In the study by Adewole et al., females accounted for 69.3% of the study population.18 The difference recorded in these studies could be due to higher number of male populace than females19 or a reflection of better health seeking habits among the males in the South-South geo-political zone of Nigeria.
The mean age of the study subjects recorded in this study was 66.8 ± 5.7 years. This figure is comparable but slightly higher than the one recorded in the study by Ogunbode et al. who reported a mean age of 69.3 ± 7.1 years among elderly patients attending a geriatric center in Ibadan comprising of 40.3% male subjects and 59.7% female subjects.20 Among the study participants, 65.9% of subjects were married, while the others were not married (single, divorced or widowed). In family types, 84.1% were monogamous, 13.1% polygamous while 2.8% practiced the extended family type. Monogamy is mostly practiced in Akwa Ibom state where the study location was situated. Most of the respondents (54.2%) were of Ibibio ethnicity, while the least ethnic group was Hausa (0.5%). This is not surprising as the Ibibio ethic group is the largest tribe in Akwa Ibom state of Nigeria.19 The percentage of study subjects who lived in the urban area was 49.5% while 50.5% lived in the rural area.
Among religion groups, 98.1% of the study subjects were Christians and only 0.5%, Muslim. In contrast, in a study by Nuhu et al. among primary care attendees in Kaduna Northern Nigeria, 51.9% of the study participants were Muslims.21 This may be due to the fact that the study area is predominantly a Christian denominated populace while Northern Nigeria is predominantly a Muslim denominated populace. Majority of the respondents (75.2%) had at least attained the primary level of education. This is slightly higher but comparable with the findings by Morgan et al. in a study among the elderly in Uyo who found the prevalence of 74.8% of those with at least one level of formal education.22 This is a usual pattern in Southern States of Nigeria where education has been free for a long time and educational attainment is a measure of accomplishment.
The overall prevalence of sleep problem in this study was 64.5%. This figure is higher than the prevalence of sleep disorders among residents aged >60 years in Northern and Southern Chinese urban areas which were 37.8% and 41.5% respectively. The figure is also higher than the reported prevalence of 49.7% in Chinese elderly people in the rural Anhui Province, 60% in Korean older adults, and 42.7% to 57.1% in Thai elderly people reporting problems with sleep.23-26 The prevalence of sleep problem in this study is however lower than the 69% reported by Adewole et al. among adults attending a Family Medicine clinic in South-West Nigeria.18
The difference observed in these studies may be due to the effect of different ethnicity and races. In this study the population was homogenous and black while the others were conducted among Asians. Environmental differences may also be responsible as these studies were done in different social settings. This may suggest ethnicity or race as a predisposing factor for sleep disorders and it has been shown that the black race has a higher prevalence of sleep disorders compared with Asians. Another factor that may be responsible for the differences in prevalence values may be the different sample sizes and study techniques used in the various studies.
In the study respondents with sleep problems, the pattern of sleep problem was early awakening with inability to sleep again (50.5%), difficulty initiating sleep (41.6%), difficulty maintaining sleep (41.6%), non-restorative sleep (38.3%) and daytime sleepiness (35.5%). These figures for early awakening, difficulty initiating and difficulty maintaining sleep are lower than the reports in the study by Lasisi and Gureje in a study among community elderly subjects with tinnitus but comparable.27 They reported 64.3% early awakening with inability to sleep again, 70.0% difficulty initiating sleep and 73.4% difficulty maintaining sleep. The prevalence for non-restorative sleep (38.3%) and daytime sleepiness (35.5%) recorded in this study is however higher than the 35.1% non-restorative sleep and 34.7% daytime sleepiness.27 The difference could be due to the larger study size and longer duration of the study. Also, the study by Lasisi and Gureje was a community study.27
On the other hand, the sleep pattern figures in this study are higher compared to an epidemiological survey performed in Japan which reported the prevalence of difficulty maintaining sleep as 15%, difficulty in initiating sleep as 8.3%, and early morning awakening prevalence of 8.0%.2 According to our study findings, the most prevalent sleep problem pattern was early morning awakening, followed by difficulty in initiating sleep and difficulty in maintaining sleep. This is different from findings by Allah et al., in a study in Egypt who reported the difficulty in initiating sleep as the most prevalent pattern of sleep problems (58.4%) followed by difficulty in maintaining sleep (53.5%) and early morning awakening (26%).28
Taking a holistic view of all related reports on sleep problem patterns, the figures from the various studies though different, agrees with the known fact that the ability to initiate and maintain nighttime sleep declines with aging. Also, sleep becomes fragmented with aging and with more nighttime awakenings leading to greater tendency for daytime sleepiness. Differences in study techniques and variations in sociodemographic conditions may be the reasons for the variations in prevalence rates across regions. With the growing population of older persons, the importance of sleep for the overall health and well-being of the elderly cannot be overemphasized. Even though this was a hospital-based study, the high prevalence of sleep problems in older persons in this study is an indication that clinicians as well as those caring for the older person should pay attention to their sleep and sleep patterns with a view to improving the overall quality of life.
References
- Safarzade S, Tohidinik H. Investigating sleep quality and epidemiology of sleep disorders in adolescents. J Res Health. 2019; 9(6):471-479.
- Buysse DJ. Sleep Health: Can We Define It? Does It Matter? Sleep. 2014;37(1): 9–17.
- Medic G, Wille M, Hemels MEH. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017; 9:151-161.
- Watson NF, Badr MS, Belensky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med. 2015;11(6):591-592.
- Carley DW, Farabi SS. Physiology of Sleep. Diabetes Spectr. 2016; 29(1):5-9.
- Brain Basics: Understanding sleep. Available at https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep.
- Becker N, Jesus SN, Marguilho R, Vistula J, Rio KA, Bella-Casal G. Sleep quality and stress: a literature review. Adv Res Heal Educ Soc Sci Towar a better Pract. 2015;(April 2016):53-61.
- Carleton EL. Sleep well, work well: Three studies. Available at http://qspace.library.queens.ca/handle/1974/13849?show=full”.
- Naja S, Makhlouf MME, Chenab MA. An ageing world of the 21st century: a literature review. Int J Community Med Public Health. 2017;4(12):4363-4369.
- Gardie A, ShaftoM, Leng Y, Kievit RA, Can C. How are age-related differences in sleep quality associated with health outcomes? An epidemiological investigation in a UK cohort of 2406 adults. BMJ open. 2017;7: e01492(1-13).
- Animasahun VJ, Chapman HJ. Psychosocial health challenges of elderly in Nigeria: a narrative review. Afri Health Sci. 2017;17(2):575-583.
- Saccomano SJ. Sleep Disorders in Older Adults. J Gerontol Nurs. 2014;40(3):38-45
- Landry GJ, Best JR, Liu-Ambrose T. Measuring sleep quality in older adults: a comparison using subjective and objective methods. Front Aging Neurosci. 2017; 7:166.
- Gulia KK, Kumar VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. 2018;18(3):155-165.
- Araoye MO. Research Methodology with Statistics for Health and Social Sciences. In: 1st ed. Ilorin: Nathadex;2004. p.115-121.
- Awokola BI, Ochayi E, Oladele S, Ogundele O, GiebelHN. C64 Upper airway and respiratory control during sleep and non-pulmonary sleep disorders: Quantification of Subjective Sleep Quality Among Elderly Patients accessing care in a family practice clinic in South-Western Nigeria. Am J Respir Crit Care Med. 2014; 189:1.
- Megbelayin EO, Babalola YO. Health Seeking Behaviours of Patients Attending Primary Eye Care Centre in Nigeria. Open Access Library Journal. 2015; 2:e1489.
- Adewole O. Sleep disorders among patients in a Nigerian Family Practice Population. Ann Med Health Sci Res. 2017:7:23-31.
- Government of Akwa Ibom State. Available at https://akwaibomstate.gov.ng/about-akwa-ibom/
- Ogunbode AM, Adebusoye LA, Olowookere OO, Owolabi M, Ogunbiyi A. Factors associated with insomnia among elderly patients attending a geriatric centre in Nigeria. Curr Gerontol Geriatr Res. 2014;2014(780535):1-10
- Nuhu FT, Yusuf AJ, Adeyemi SO, Kalu AO. Sleep quality among primary care attendees in Kaduna, Northern Nigeria: A case-control study. Int J Psychiatry Med. 2013; 46(3):291-301.
- Morgan UOM, Etukumana EA, Abasiubong F. Sociodemographic factors affecting the quality of life of elderly persons attending the general outpatient clinics of a tertiary hospital, South-South Nigeria. Niger Med J. 2017; 58:138-142.
- Thichumpa W, Howteerakul N, Suwannapong N, Tantrakul V. Sleep quality and it’s contributing factors among elderly living in rural Chiang Rai, Northern Thailand. Epidemiol Health. 2018;40: e2018018.
- Li J, Yao YH, Dong Q, Dong YH, Liu JJ, Yang LS, et al. Characterisation and factors associated with sleep quality among rural elderly in China. Arch Gerontol Geriatr. 2013; 56(1):237-243.
- Park J, Yoo M, Bae SH. Prevalence and predictors of poor sleep quality in Korean older adults. Int J Nurs Pract. 2013; 19(2):116-123.
- Wang P, Song L, Wang K, Han X, Cong L, Wang Y, et al. Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area; a population study. Aging Clin Exp Res 2020; 32:125-131.
- Lasisi AO, Gureje O. Prevalence of Insomnia and impact on quality of life among community elderly with Tinnitus. Ann Otol Rhinol Laryngol. 2011;120(4):226-230.
- Allah ESA, Abdel-Aziz HR, El-Seoud ARA. Insomnia: Prevalence, risk factors, and its effect on quality of life among elderly in Zagazig City, Egypt. J Nurs Edu Pract. 2014;4(8);52-69.