A seven-year review of paediatric mortality in the University Of Uyo Teaching Hospital, Uyo, Nigeria
Akpan UM, Ekpenyong EE, Dickson AJ, Oloyede IP
Abstract
Background: Childhood mortality has become one of the world’s targets for reduction as encapsulated in the Sustainable Development Goals (SDG). Although mortality among children aged younger than 5 years has declined globally in the past two decades, considerable geographical differences exist and remain disproportionately high in sub-Saharan Africa and Southeast Asia. Many hospital-based studies in Nigeria have shown the predominance of infectious diseases such as sepsis, bronchopneumonia, and HIV/AIDS as the leading causes of childhood mortality.
Methods: The study was conducted at the Department of Paediatrics of the University of Uyo Teaching Hospital (UUTH), Uyo, Akwa Ibom State, Nigeria. The study was a descriptive, cross-sectional and retrospective review of all the deaths among the hospitalized children from 1st January 2015 to 31st December 2021.
Results: A total of 191 deaths in the Paediatrics Department of the University of Uyo Teaching Hospital were recorded, 99 males (51.3%) and 92 females (47.7%). This study shows that 27.00% of children who died where infants, 28.30% were children 1-5 years and 44.50% were children above 5 years. The commonest cause of childhood mortality in this study was severe sepsis (30.00%), followed by HIV/AIDS (11.40%), bronchopneumonia (9.84%).
Conclusion: Most of the leading causes of childhood mortality in Nigeria are infectious diseases. These are largely preventable and leave room for improvement in our practice of Infection Prevention and Control (IPC), appropriate community education on hygienic practices and prevention of HIV/AIDS.
Introduction
Childhood mortality refers to the death of a child. It has become one of the world’s targets for reduction since the era of the Millennium Development Goals (MDG) to the Sustainable Development Goals (SDG).1,2 The target of SDG for the child in all countries is to achieve an under-5 mortality rate (U5MR) of 25 or fewer deaths per 1000 livebirths by 2030, (SDG target 3.2.1) and a neonatal mortality rate (NMR) of 12 or fewer deaths per 1000 livebirths by 2030 (SDG target 3.2.2).1,2
In 2015, Sub-Saharan Africa and South Asia collectively accounted for 81% of the 5.9 million under-5 deaths and 77% of the 2.6 million stillbirths worldwide.4 Although mortality among children aged younger than 5 years has declined globally in the past two decades, considerable geographical differences exist. Child mortality remains disproportionately high in sub-Saharan Africa and Southeast Asia.
Older children and adolescents (aged 5–19 years) are said to make up a quarter of the world population.4 Thus, investments in the survival and health of children in this age group will bring threefold benefits of improving their health now, their future health, and the health of the next generation. However, studies have reported that 1·48 million deaths occurred in this age group globally in 2019 and nearly all of these from preventable causes.2 Following the achievements made in reducing mortality in children younger than 5 years between 2000 to 2015, the survival of older children and adolescents has gained attention.3,4
In a 10 – year systematic review, Liu, L. et al5 grouped the causes of childhood mortality into eight categories, including pneumonia, diarrhoea, meningitis, injury, malaria, congenital abnormalities, causes arising during the perinatal period, and other causes. Death caused by severe malnutrition were grouped separately in that study. Out of 7.6 million under 5 mortality in 2010, 64·0% died of infectious causes with pneumonia (18·3%), diarrhoea (10·5%), and malaria (7·4%) leading. About 40% occurred in the neonatal period, most often due to preterm birth complications (14·1%), intrapartum related complications (9·4%), and neonatal sepsis or meningitis (5·2%). Congenital abnormalities (3.5%) and injury (4.6%) were also important causes in that study.
Perin et al6 in 2021 reported that an estimated 5.30 million children died before reaching their fifth birthday. This marked a significant decrease from the estimated 9.92 million under 5 deaths in 2000. This decline was considered to be a result of collaborative efforts across various organizations and governments during the Millennium Development Goals (MDGs) era from 2000 to 2015, and in the subsequent period of the Sustainable Development Goals (SDGs), representing a decline in under-5 mortality rate from 75 deaths per 1000 livebirths in 2000, to 38 deaths per 1000 livebirths in 2019. However, despite such an extraordinary reduction, the global under-5 mortality rate is still well above the target of 25 deaths per 1000 livebirths as defined by SDG 3.2.3,6 In this study, the leading causes of death were preterm birth complications (17·7%), lower respiratory infections (13·9%), and intrapartum-related events (11·6%), constituting 43·2% of under-5 deaths. Vaccine-preventable deaths, such as for lower respiratory infections, meningitis, and measles, constituted 21·7% (20·4–25·6) of under-5 deaths. Nigeria is among the ten countries in the world with the highest number of under-5 deaths, with India, Pakistan, Democratic Republic of the Congo, Ethiopia, China, Indonesia, Tanzania, Bangladesh, and Angola in that category. Together, these ten countries have 3·15 million under-5 deaths, which represents 59·5% of the global burden.6
In 2019, Nannan et al7 reviewed the mortality trends and causes of death in South Africa between 1997 to 2012. Under-5 mortality per 1000 live births increased from 65 in 1997 to 79 in 2004 as a result of HIV/AIDS, before dropping to 40 by 2012. The death rate from diarrhoeal diseases began to decrease in 2008 and the death rate from pneumonia from 2010. The study posited that as at 2012, neonatal deaths accounted for 27% of child deaths, with conditions associated with prematurity, birth asphyxia and severe infections being the main contributors. This variation in the causes of mortality is true both between countries and between states in a country. They emphasized that prevention of mother-to-child transmission of HIV, the Expanded Programme on Immunisation and programmes aimed at preventing neonatal deaths needed to be equitably implemented throughout the country to address persistent provincial inequalities in child deaths.
In a Port Harcourt Nigeria in a two year retrospective study of the mortality pattern in children admitted to the children’s ward in University of Port Harcourt Teaching Hospital in 2009, noted that 80.3% death were in children under 5 years of age with HIV/AIDS as the leading cause.
While in Umuahia, South East Nigeria in 2014, it was highlighted that malaria was the leading cause of mortality beyond the neonatal period.10 Other common mortality causes were pneumonia, septicaemia, diarrhea, HIV AIDS and meningitis each accounting for 10%, 10%, 7%, 7% and 5% respectively.10
Similarly in Bayelsa, South South Nigeria, in 2021, most deaths were seen in children less than 5 years of age (82.7%). The common causes of death were septicaemia (34.8%) and severe malaria (34.8%) among the under-fives and meningitis (25.0%) and HIV/ TB (20.8%) among those above the age of 5 years.11
In the University of Uyo Teaching Hospital, a previous assessment was carried out by Ijezie and Okpokowuruk13 in 2016 reviewing all deaths in hospitalized children in the department of Paediatrics, University of Uyo Teaching Hospital between January 2009 and December 2014 in a retrospective cross-sectional descriptive study. More than half of the deaths were neonatal deaths with prematurity (38.7%) and birth asphyxia (19.4%) leading. In infants, bronchopneumonia and septicaemia 33% and 27.5% respectively were the leading causes. Malaria (23%) and bronchopneumonia (25%) accounted for most deaths in children aged 1 to 5 years of age. While malignancies lead in older children, followed by septicaemia (0.7%).13 They concluded that childhood mortality remained high, emphasizing the necessity for ongoing advocacy efforts at both facility and community levels with the aim of enhancing awareness and care-seeking behavior among parents and caregivers, alongside improvements in hospital practices, to benefit the overall well-being of children.
This study aimed to evaluate the mortality pattern in children admitted into the Department of Paediatrics, University of Uyo Teaching Hospital, Uyo, Akwa Ibom State, Nigeria.
Materials and methods
The study was conducted at the Department of Paediatrics of the University of Uyo Teaching Hospital (UUTH), Uyo, Akwa Ibom State, Nigeria. The University of Uyo Teaching Hospital is the only tertiary hospital located in Uyo, Akwa Ibom State and therefore the only referral centre owned by the federal government. The study was a descriptive, cross-sectional and retrospective review of all the deaths among the hospitalized children from 1st January 2015 to 31st December 2021. The diagnosis of the disease entities were done by the paediatricians who attended to the patients on the basis of the clinical features and the laboratory results that were obtained. The data of all children who died within the period under review were studied and relevant information extracted including age, sex, date and time of admission, date and time of death, and diagnosis. The statistical analysis was done using basic descriptive statistics.
Results
Table 1: Comparing ages and duration of stay of children before death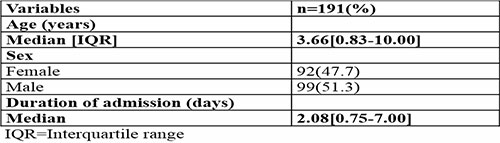
Table 2: Comparing sex and duration of hospital stay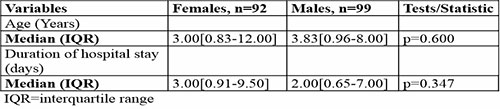
Within the period under review, there were 191 deaths in the Paediatric Department of the University of Uyo Teaching Hospital, 99 males (51.3%) and 92 females (47.7%).
Median age at demise was 3.66days (IQR = 0.83 – 10.00).
Figure 1 below shows the distribution of mortality pattern. First year reviews shows 9.80% mortality while the centre recorded the highest childhood mortality in 2019 at 25.40%.
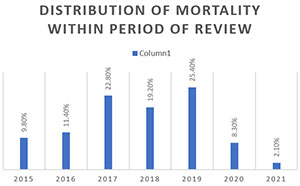
Figure 1: Distribution of mortality between 2015 and 2021
Figure 2 below shows the distribution of mortality based on sex. In 2015, 52.60% of males died compared to 47.40% of females. By 2021, 75.00% of those that died were males and 25.00% females.
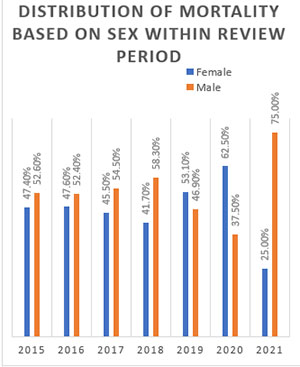
Figure 2: Distribution of mortality based on Sex
Figure 3 below shows the age distribution of childhood mortality. This study shows that 27.00% of children who died where infants, 28.30% were children 1-5 years and 44.50% were children above 5 years.
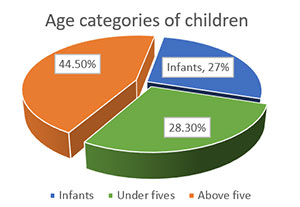
Figure 3: Age and mortality distribution in children
The commonest cause of childhood mortality in this study was severe sepsis (30.00%), followed by HIV/AIDS (11.40%), bronchopneumonia (9.84%).
Other common causes of childhood mortality were: neoplastic diseases (8.81%), diarrhoea diseases (8.29%), and neurologic diseases (7.25%).

Figure 4: Common causes of childhood mortality
Discussion
This study shows that one hundred and ninety-one childhood mortality occurred within the period under review. When compared to the review by Ijezie et al13 in the same centre, this review had a lower mortality. This may have been attributed to the inclusion of neonates with higher mortality in the previous review, and possible improvement in management protocols of common illnesses during our study period.
More male children died than female (99:92) though not statistically significant in this study. This may have been attributed to the importance placed on male children in African culture culminating in better healthcare seeking behaviour for them compared with their female counterpart, and may represent underreporting of female mortality since they may occur more at home.
This retrospective review shows the peak of childhood mortality in the centre to be around 2017 to 2019 followed by a decline in 2020 and 2021. This decline may have been due to the COVID-19 pandemic with a decline in global hospital attendance during the lockdown, thus, fewer hospital admissions were recorded. It was also reported that children did not have high mortality due to COVID-19 because the diseases were mostly mild.14
This study showed that under-5 mortality is still higher than mortality in older children at the University of Uyo Teaching Hospital. This was corroborated by Perin et al,6 Liu et al5 and Ijezie et al.13 The similarity noticed may be due to the well-recognized higher frequency of infections in children under 5 years of age due to their lower immune system.3
Overall, the leading cause of childhood mortality within the period under review was severe sepsis followed by HIV/AIDS. Others in order of causing mortality are: bronchopneumonia, malignancies (such as nephroblastoma, retinoblastoma and acute lymphoblastic leukemia), diarrhoea disease, and malaria. These findings were similar to the findings of Ijezie et al13 in the same centre in 2016 where they did a retrospective review of the mortality pattern from 2009 to 2014. They found septicaemia as the leading cause in children one month and above. This review saw HIV/AIDS as the second commonest cause of mortality as against bronchopneumonia found by Ijezie et al13 in the same centre. The two reviews were a retrospective study which may be the reason for similar leading cause of mortality. Sepsis as the leading cause may be due to increasing antibiotics abuse in our environment, misdiagnosis of all fever as malaria in lower healthcare settings, increased poverty and poor hygiene. The difference in the second commonest cause may be attributed to the increased awareness and case finding for HIV which has allowed for displacement of bronchopneumonia in this study to the third position. Other reasons for the prominence of HIV/AIDS in this study may be due to poor adherence in the treatment due to dependence on caregivers for drug administration.
Similarly, this finding was corroborated by Duru et al11 in 2021 when they reviewed the childhood mortality record at Niger Delta University Teaching Hospital, Bayelsa State where septicaemia was the leading cause of childhood mortality followed by severe malaria and meningitis. This similarity further buttress the fact that infections remain the highest contributor to childhood mortality in Nigeria.
However, this was in contrast with the findings of George, Alex-Hart and Briggs in 20099 in a similar review of childhood mortality at the University of Port Harcourt Teaching Hospital in which HIV/AIDS was the commonest cause of childhood mortality followed by bronchopneumonia. There are other contrasting findings of the commonest cause of childhood mortality as found in Nwafor et al,10 Perin et al6 and Nannan et al.7 Nwafor et al10 in 2014 at the Federal Medical Centre Umuahia found the leading cause of childhood mortality to be malaria, followed by pneumonia and septicaemia. Perin et al6 in 2019 while assessing the common causes of under-5 mortality in some African countries including Nigeria, found pneumonia, diarrhoea and malaria in that order. Nannan et al7 in 2019 in South Africa in a similar study discovered HIV/AIDS as the leading cause of childhood mortality followed by diarrhoea and pneumonia. These findings though in contrast to the findings in this study still showed infections as the leading cause of childhood mortality. The differences in the specific causes of mortality may have been due to differences in the peculiarities of diagnosis of sepsis in different centres and probably increased case finding of HIV.
Conclusion
Despite the reported decrease in childhood mortality around the world, regional disparities occur with sub-Sahara Africa and Southeast Asia still having a high proportion of childhood mortality. Most of the leading causes of childhood mortality in Nigeria are caused by infectious agents and septicaemia has been identified in this study as the commonest cause followed by HIV/AIDS and bronchopneumonia. These are largely preventable causes and leave room for improvement in our practice of Infection Prevention and Control (IPC), appropriate community education on hygienic practices and prevention of HIV/AIDS.
References
- The Inter-Agency Group for Child Mortality Estimation (IGME). Estimates of under-five mortality rates by country, the 2011 release. www.childmortality.org.
- Sharrow D, Hug L, You D, Alkema L, Black R, Cousens S, et al. Global, regional, and national trends in under-5 mortality between 1990 and 2019 with scenario-based projections until 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. The Lancet Global Health. 2022 Feb 1;10(2):e195-206.
- UN. The millennium development goals report 2010. New York: United Nations, 2010.
- UNICEF, WHO, World Bank, UN Population Division. Levels and trends in child mortality report 2011: estimates developed by the Inter-agency Group for Child Mortality Estimation. http://www. childinfo.org/fi les/Child_Mortality_Report_2011.pdf
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. The lancet. 2012 Jun 9;379(9832):2151-61.
- Perin J, Mulick A, Yeung D, Villavicencio F, Lopez G, Strong KL, et al. Global, regional, and national causes of under-5 mortality in 2000–19: an updated systematic analysis with implications for the Sustainable Development Goals. The Lancet Child & Adolescent Health. 2022 Feb 1;6(2):106-15.
- Nannan NN, Groenewald P, Pillay-van Wyk V, Nicol E, Msemburi W, et al. Child mortality trends and causes of death in South Africa, 1997-2012, and the importance of a national burden of disease study. South African Medical Journal. 2019 Jul 1;109(7):480-5.
- Adedokun ST, Yaya S. Childhood morbidity and its determinants: evidence from 31 countries in sub-Saharan Africa. BMJ Global Health. 2020 Oct 1;5(10):e003109.
- George IO, Alex-Hart BA, Frank-Briggs AI. Mortality pattern in children: A hospital based study in Nigeria. International journal of biomedical science: IJBS. 2009 Dec;5(4):369.
- Charles NC, Chuku A, Anazodo NM. Childhood mortality in Federal Medical Centre Umuahia, South eastern Nigeria. Oman Med J. 2014 Sep;29(5):320-4.
- Duru C, Paul NI, Peterside O, Akinbami F. Pattern of mortality among Childhood emergencies at the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. Nigerian Journal of Paediatrics. 2019;46(2):55-60.
- Odejimi A, Quinley J, Eluwa GI, Kunnuji M, Wammanda RD, Weiss W, et al. Causes of deaths in neonates and children aged 1–59 months in Nigeria: verbal autopsy findings of 2019 Verbal and Social Autopsy study. BMC Public Health. 2022 Jun 6;22(1):1130.
- Ijezie E, Okpokowuruk FS. Mortality audit in the paediatrics department of the University of Uyo teaching hospital, Uyo, Nigeria. Int J Res Med Sci. 2016;4(2):615-20.
- Ekpenyong EE, Akpan UM, Oloyede IP, Ekanem AM, Umoette N, Peters E. Spectrum of COVID-19 infection in children in Southern Nigeria. Nigerian Journal of Paediatrics. 2022 May 2;49(1):17-21.