Effect of chronic formaldehyde exposure on some pulmonary functions among medical students in a tertiary institution in Edo State, Nigeria
Ebojele FO*, Iyawe VI
Abstract
Background: The effect of formaldehyde exposure on some pulmonary functions among medical students in a tertiary institution in Edo State, Nigeria was studied.
Materials and Methods: 150 subjects were studied which was divided into three groups A, B, and C with 50 subjects in each group. Group A served as control with nil exposure while groups B and C served as the test groups with 0-9 months exposure and 10-18 months exposure respectively. The pulmonary functions measured included Respiratory Rate, Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 second (FEV1), FEV1/FVC ratio, Peak Expiratory Flow Rate (PEFR) and Forced Expiratory Flow (FEF25-75) and these were obtained with the aid of a digital spirometer. Test results were given as measured values in litres and as percentages of predicted values. Statistical analysis was done using Graph Pad Prism version 5.0. Results were presented as Mean ± SEM. Analysis of Variance was used to compare the means of test and control values while post hoc test was done using Student Newman Keul’s test and a P-value of less than 0.05 was considered as statistically significant.
Results: Results showed significant decrease in FEV1, FEV1/FVC, PEFR and FEF25-75. However, there was a significant increase in Respiratory Rate.
Conclusion: It was therefore concluded that exposure to formaldehyde has deleterious effects on the respiratory health of medical students.
Keywords: formaldehyde, medical students, pulmonary function, exposure
Introduction
In the course of training, medical students in addition to other laboratories are required to pass through the Anatomy laboratory where formaldehyde is freely used.1 Formaldehyde is used to fix tissues which are relevant for microscopic as well as histological studies.2 It is also important in embalming human and animal remains thereby preventing them from undergoing decomposition as well as helping the bodies to retain the normal anatomical relations thereby making it easy for the purpose of study during anatomy dissections in medical schools.2,3 Attention has been drawn to formaldehyde with regard to its possible health hazards. Some published reports have suggested that exposure to formaldehyde could be associated with adverse effects on the respiratory health.4 Available studies on acute occupational exposure in humans revealed clinical symptoms like skin irritation, eye soreness, nose irritation, throat irritation and rhinorrhea as well as reduction in pulmonary function like FVC, FEV1/FVC, and PEFR.5,6,7,8 It has also been reported that formaldehyde inhalation may produce or exacerbate allergic effects and asthma in children and adults.9,10 The aim of this study was to ascertain the effect of formaldehyde exposure on some pulmonary functions among medical students in a tertiary institution in Benin City, Nigeria.
Materials and methods
Medical Students of a tertiary institution in Edo State, Nigeria between the ages of 18-30 years were recruited for this study. Subjects were apparently healthy, non-smokers, and had no history of cardiopulmonary disease or recent abdominal or chest surgery. Informed consent was obtained from the subjects who participated in the study while ethical approval was obtained from the College Research Ethics Committee, University of Benin before commencement of the work. Subjects were divided into three groups A, B and C with fifty subjects in each group. Group A served as control (non-medical students with nil exposure to formaldehyde) while groups B and C served as the test group. Group B consisted of medical students with 0-9 months exposure to formaldehyde in the Anatomy laboratory while Group C consisted of medical students with 10-18 months exposure to formaldehyde in the Anatomy laboratory. The Respiratory Rate was counted for one minute in all the subjects by simple observation of the chest movement during respiration. Other pulmonary functions measured included Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 second (FEV1), FEV1/FVC ratio, Peak Expiratory Flow Rate (PEFR) and Forced Expiratory Flow (FEF25-75) and these were obtained with the aid of a digital spirometer (Hygeia). Test results were given as measured values in litres and as percentages of predicted values. The tests were carried out after a detailed explanation of the procedure to the subjects. Each subject was instructed on the need to put in maximum effort at blowing into the instrument. Each subject was asked to adopt a sitting position and thereafter place the mouth piece of the spirometer tightly around the mouth to prevent leakage of air. The subject was then asked to inspire maximally and then exhale forcefully through the mouth into the spirometer. Three trials were done for each subject and the best of the three readings was selected. This is as described by the American Thoracic Society in 199511. Statistical analysis was done using Graph pad prism version 5.0. Results was presented as Mean ± SEM. Analysis of Variance was used to compare the means of test and control values while post hoc test was done using Student Newman Keul’s test and a p-value of less than 0.05 was considered as statistically significant.
Results
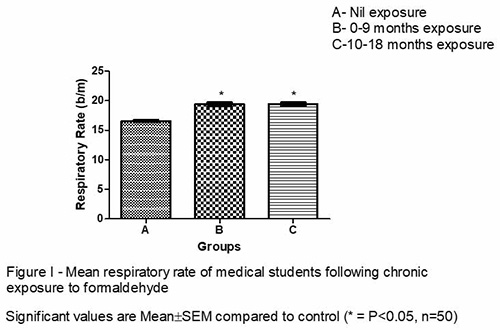
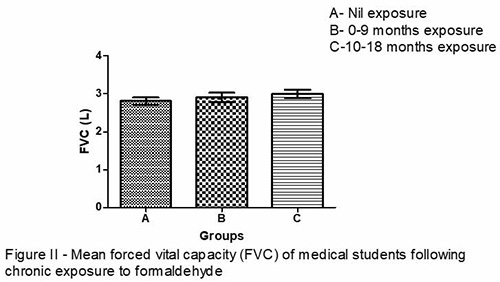
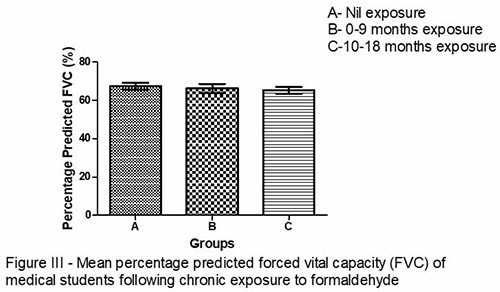
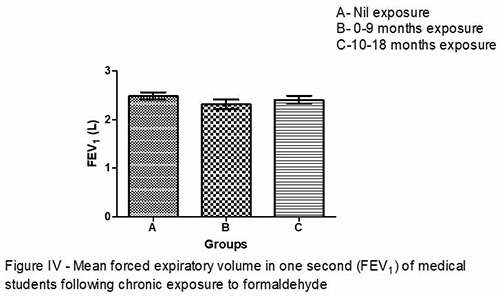
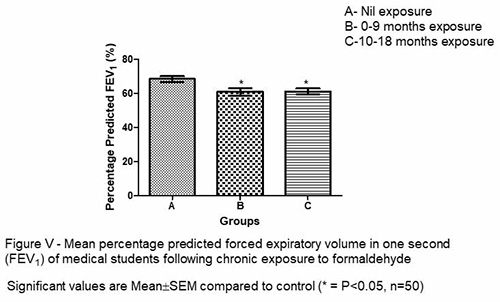
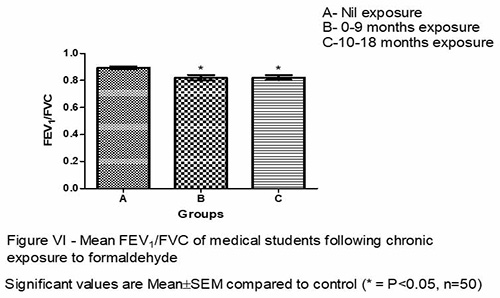
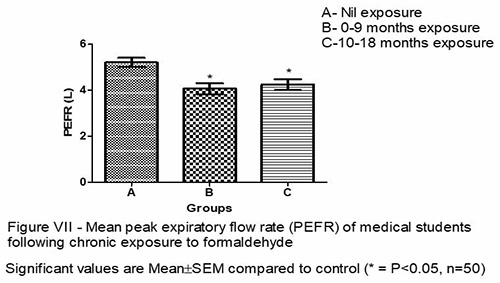
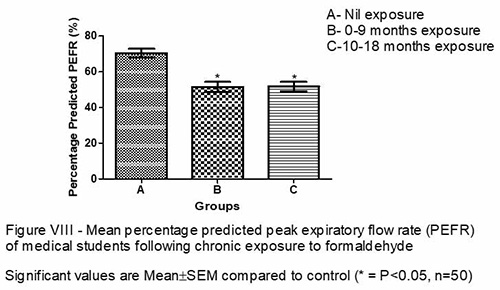
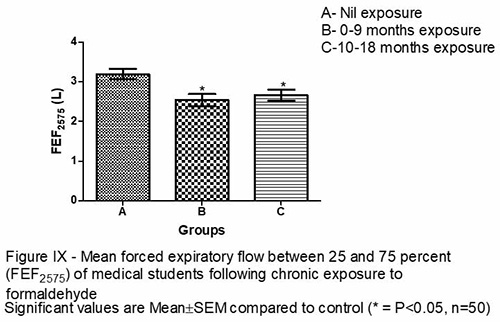
Respiratory Rate (figure I) was significantly higher in groups B and C when compared with the control. Figures II and III revealed an observable decrease in FVC in groups B and C when compared with the control. There was an observable decrease in FEV1 in groups B and C when compared with the control as shown in figure IV and a significant decrease was reflected in the percentage predicted FEV1 in figure V. FEV1/FVC ratio was significantly reduced in groups B and C when compared with the control (figure VI) while PEFR and FEF25-75 (figures VII, VIII and IX) were significantly lower in groups B and C when compared with the control.
Discussion
Respiratory rate was significantly increased in both groups B and C when compared to the control (Figure I). The possible mechanism of this increase may have been as a result of sensory irritation along the airway which may have caused irritant receptors within the airway to bring about reflex bronchospasm and tachypnea 12 hence reducing the quantity of formaldehyde that is getting into the lungs. Irritant receptors send impulses to the respiratory centre through the vagus nerve and in the pons the pneumotaxic centre is known to increase respiratory rate by decreasing the duration of inspiration.12 FEV1 and FEV1/FVC were significantly reduced (Figures V and VI) indicating that there is airway obstruction. FEF25-75 was also significantly reduced (Figure IX) showing that there is obstruction of the smaller airways. PEFR was significantly reduced (Figure VII) indicating that there is obstruction of both the medium and smaller airways. These reduction in lung function indices are consistent with the findings of some other researchers such as Khamgaonkar and Fulare5 who reported reduction in FVC, FEV1/FVC and Maximum Expiratory Effort. Pourmahabadian et al.7 reported reduction in FVC and FEV1 while a decrease in PEFR was reported by Kriebel et al.13 and Neginhal et al.14 These reduction are also consistent with the findings of Patil et al.15 and Shrivastava and Saxena.16 In this present study, the possible mechanisms by which formaldehyde may have caused the reduction in lung function parameters could have been through the irritant receptors bringing about reflex bronchospasm that could have narrowed the airway thereby causing obstruction.12 It could also have been as a result of inflammation as inflammatory cells, when activated are known to release certain chemical mediators like leucotrienes that can cause bronchoconstriction as well as increase in mucus production that are capable of clogging and narrowing the airways.17 Again, it is possible that the increase in mucus production may have been overwhelming such that the mucociliary clearance mechanism was unable to cope with the clearance rate and there is a resultant clogging and narrowing of the airway by excess mucus. Another possible mechanism may have been a complete failure of the mucociliary clearance mechanism itself owing to tissue destruction.18 Chronic inflammatory cells are known to elaborate proteases that are capable of damaging bronchial tissues and the cilia could have been damaged.
Following the observations from this study we therefore conclude that there is a need to find ways of reducing the atmospheric level of formaldehyde within the Anatomy laboratory by introducing proper ventilation system, air extractors and formalin adsorbers in the dissection hall. Other alternative fixatives like Gluteraldehyde, Phenoxyethanol, and Kryofix can also be used in place of formaldehyde while Students should be encouraged to use personal protective equipment like facemask in order to protect their respiratory health.
References
- Obikili E.N, Esom E.A, Ezepue U.F. Performance of students in Anatomy in the 2nd MBBS examinations. Orient J Med 2006; 18(1&2):11-15.
- Farooqui M. Y. H. Formaldehyde. J Appl Toxicol 1983; 3: 264-265.
- IARC monographs on the evaluation of carcinogenic risks to humans. Vol. 88. Formaldehyde, 2-butoxyethanol and 1-tert-butoxypropan-2-ol. Geneva, Switzerland: International Agency for Research on Cancer 2006; 39-93, 273.
- Mathur N, Rastogi S.K. Respiratory effects due to occupational exposure to formaldehyde; systematic review with meta analysis. Indian J Occup and Environ Med 2007; 11: 26-31.
- Khamgaonkar M.B, Fulare M.B. Pulmonary effects of formaldehyde exposure - an environmental epidemiological study. Indian J Chest Dis Allied Sci 1991; 33: 9-13.
- Kim H, Kim Y, Cho S. Formaldehyde exposure levels and serum antibodies to formaldehyde-human serum albumin of Korean medical students. Arch Environ Health 1999; 54(2): 115-118.
- Pourmahabadian M, Azam K, Ghasemkhani M. Pulmonary function study between formaldehyde exposed and non-exposed staffs at some of the Tehran educational hospitals. J Med Sci 2006; 6(4): 621-625.
- Wei C.N, Harada K, Ohmori S. Subjective symptoms of medical students exposed to formaldehyde during a gross anatomy dissection course. Int J Immunopathol Pharmacol 2007; 20(2): 23-25.
- Sakamoto T, Doi S, Torri S. Effects of formaldehyde as an indoor air pollutant on the airway. Allergol Int 1999; 48(3): 151-160.
- Mendell M.J. Indoor residential chemical emissions as risk factors for respiratory and allergic effects in children: A review. Indoor Air 2007; 17(4): 259-277.
- American Thoracic Society. Standardization of Spirometry 1994 update. Am J Resp Crit Care Med 1995; 152: 1107-1136.
- Guyton A.C, Hall J.E. Textbook of Medical Physiology. 12th edn. Philadelphia. Elsevier Saunders 2011; Pp473.
- Kriebel D, Sama S.R, Cocanour B. Reversible pulmonary responses to formaldehyde: A study of clinical anatomy students. Am Rev Respir Dis 1993; 148: 1509-1515.
- Neginhal R, Herur A, Chinagudi S, Rairam G.B, Kolagi S, Ambi U. Cardiorespiratory effects of acute exposure to formaldehyde in gross anatomy laboratory in medical students- A comparative study. Medica Innovatica 2013; 2(1): 32-35.
- Patil P, Hulke S.M, Thakare A. Effect of formalin on pulmonary function: a nine months longitudinal study. Research J of Pharmaceutical Biol and Chem Sci 2012; 3(1): 211-216.
- Shrivastava A, Saxena Y. Effect of formalin vapour on pulmonary function of medical students in anatomy dissection hall over a period of one year. Indian J Physiol Pharmacol 2013; 57(3): 255-260.
- Salmon J.A, Higgs G.A. Prostaglandins and leukotrienes as inflammatory mediators. British Medical Bulletin 1987; 43(2): 285-296.
- Ebojele F, Iyawe V. Histology of the airways following chronic exposure to formaldehyde in Wistar Rats. J Anat Sci 2022; 13(1): 96-100.